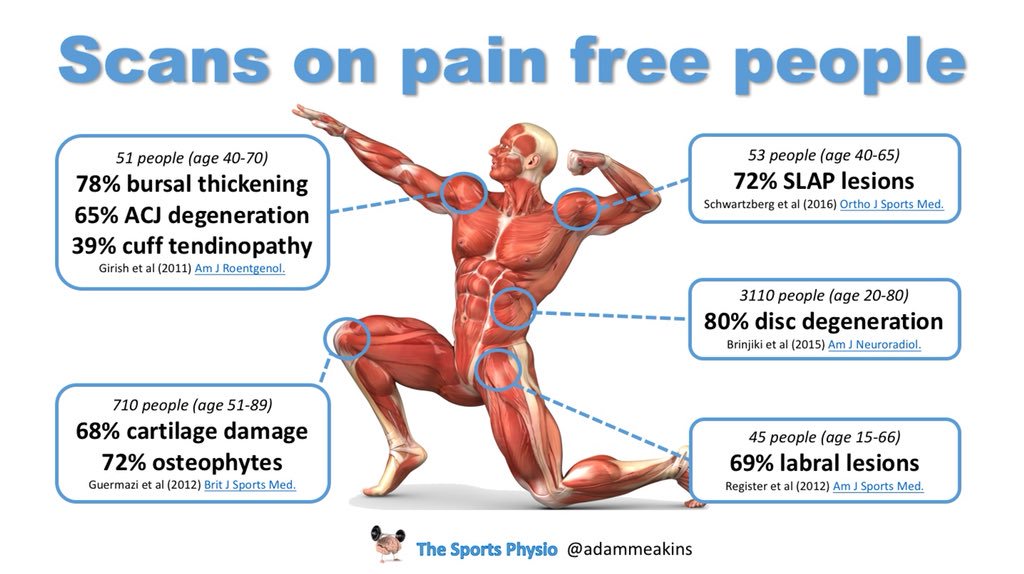
As the weeks go by I am overwhelmed by telephone enquiries with clients with prolapsed discs. Back injuries are the most common of all orthopaedic injuries and they happen in gyms and workplaces alot. This is why we assess rather than guess. Throwing clients straight into any sort of class can be detrimental to their back herniation and everyone is different. Just because your MRI shows a bulge, does NOT mean you have a disc bulge that is causing your pain, but it should be viewed as “suspect”. The 1995 (1) paper shows that 76 % of the population have all the disc protrusion, bulges etc but this did not relate to pain. The diagram below is a more updated study from 2014. It is astounding how much our society believes that all back pain is related to the disc. This is where the disc-onnect happens. Sure, the disc is one of those structures that is inherently part of the spine. But not all low back pain problems are disc problems. You may be easily mislead by MRIs. If you do not have any red flags, then consideration must be given to some other potential issues.
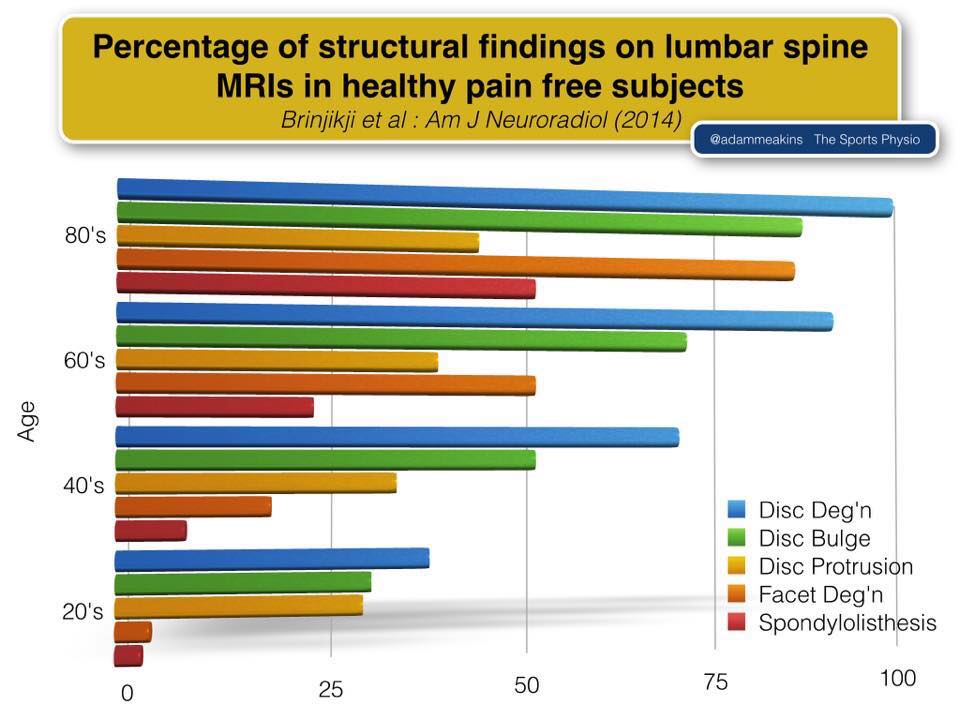
ALL of these individuals are people who DO have disc bulges, but DO NOT have PAIN. I will repeat for the sake of clarity…many of these PAIN-FREE individuals have disc bulges!
Finding the right exercise to heal
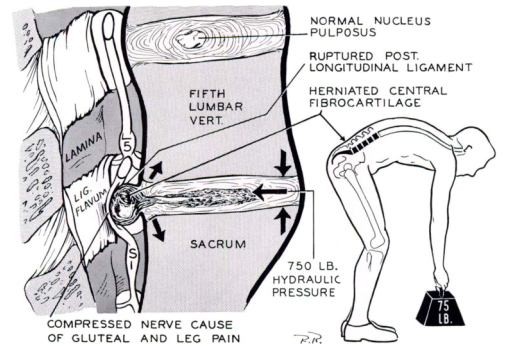
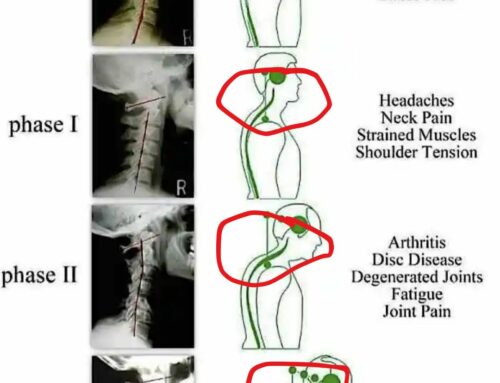
So many exercises are in flexion. This means as you bend forwards each vertebrae above slides forward on the vertebrae below. So if we think about the lumbar spine and particularly L4/L5, when bending forwards the force bends down so the disc is pushed back, but the load is being transferred. This can be reversed with an effective corrective exercise, core conditioning and lifestyle program.
The most important warning signs to watch out for are:
- Pain is worst in the morning but gets better as the day goes on (provided you are being cautious about not provoking it)
- Any degree of spinal flexion increases the pain, in particular, the referral pain down the leg
- Arching your back (lumbar extension) makes your back feel better Back feels better standing than sitting (not always the case)
- Lying face down feels like the best position
- Referred pain going to the butt or further down
Movements that must ABSOLUTELY be avoided include:
1. Flexion of the spine
2. Sidebending of the spine
3. Rotation of the spine
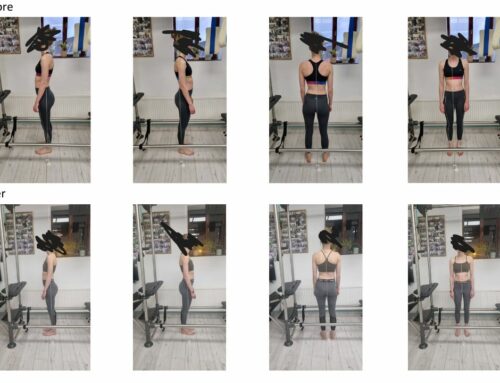
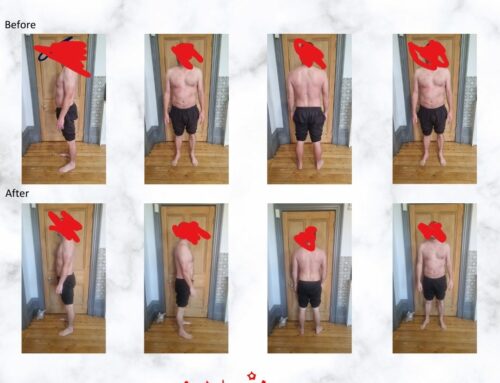
I’ve learned to have super good posture both at rest and during exercise will help structural and functional support around the disc. The spine needs to be stabilized using exercises designed to train the inner unit (TVA, multifidus, etc). When there is a disc injury it is shown that the multifidus muscles atrophy rather quickly thus reducing the stability of the injured segment. Flexibility also has to be assessed as well as weakness in the muscles that are innervated by the nerves that run out of those two segments.
Lesson number 1: Get an MRI as early as possible and keep pushing for one. I know there are studies that say it’s not a perfect diagnostic tool, but here’s just my experience: They take you much more seriously when you can visibly see the herniated disc.

Red flags
Who Should NOT Perform Exercises
If any of the following occurs, do NOT do ANYTHING without consulting your doctor first:
- If you have developed lower back pain for the first time and it is no better 10 days after onset
- If you have severe pain in the leg below the knee and you experience sensations of weakness, numbness, or “pins and needles” in a foot and the toes
- If, following a recent severe episode of back pain, you have developed bladder problems
- If you are generally feeling unwell in conjunction with the attack of lower back pain a corrective exercise programme using Pilates and Yoga help?
The first step in any exercise progression is to remove the cause of the pain, namely the perturbed motion and motor patterns. For example, the flexion intolerant back is very common in today’s society. Giving this type of client stretches such as pulling the knees to the chest may give the perception of relief (via the stimulation of erector spinae muscle stretch receptors) but this approach only guarantees more pain and stiffness the following day as the underlying tissues sustain more cumulative damage. This is why I dont give it.

Eliminating spine flexion, particularly in the morning when the discs are swollen from the osmotic super hydration of the disc that occurs with bed rest, has been proven very effective with this type of patient.
Stages of therapeutic exercise
- Corrective exercise
- Groove appropriate and perfect motion and motor patterns. Encode movement stability (mobility at some joints such as the hips and stability of the lumbar spine).
- Build whole body joint and stability (mobility at some joints such as the hips and stability of the lumbar spine)
- Increase endurance
- Build strength
- Develop speed, power, agility
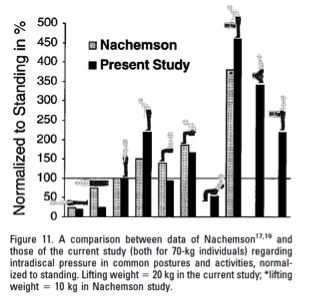
Postural changes have varying effects on lumbar disc pressure at various positions. Disc pressure and stress on the lumbar spine are at its lowest when lying in the supine position (25 kg). These stresses slightly increase when you change from the supine position to lying on your side; this disc pressure is measured at 75 kg. 100 kg of pressure is measuring on the disc of the lumbar spine when you are standing in the upright position. When a person is leaning forward from the standing position the pressure increases to 150 kg. Holding a weight and leaning forward in the standing position causes this pressure to further rise to 220 kg. A non-load bearing position of sitting upright will place 140 kg of pressure on the lumbar disc. Leaning forward from this position then raises the pressure to 185 kg. Finally, the highest pressure that is placed on the disc of the lumbar spine occurs when you are in the seated position and leaning forward, while bearing weight. The idea is to hold this weight closer to the body to reduce the pressure being placed on the discs.
Bibliography
- Boos, N., Rieder, R., Schade, V., Spratt, KF., Semmer, N., Aebi, M., 1995. Volvo Award in clinical sciences. The diagnostic accuracy of magnetic resonance imaging, work perception, and psychosocial factors in identifying symptomatic disc herniations. Spine (Phila Pa 1976). 1995 Dec 15; 20(24):2613-25.
Stuart McGill
Paul Chek “Eat, move and be healthy”
Sam Visnic – Chek coach
PT on the net
Adam Meakins – Sports Physio